Search
- Page Path
- HOME > Search
Original Article
- Analysis of pregnant women with critically severe COVID-19 in Republic of Korea from February 2020 and December 2021
- Ji Joo Lee, Sang-Eun Lee, Yeonjung Kim, Young-Joon Park
- Osong Public Health Res Perspect. 2023;14(2):129-137. Published online April 5, 2023
- DOI: https://doi.org/10.24171/j.phrp.2023.0025
- 1,295 View
- 58 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 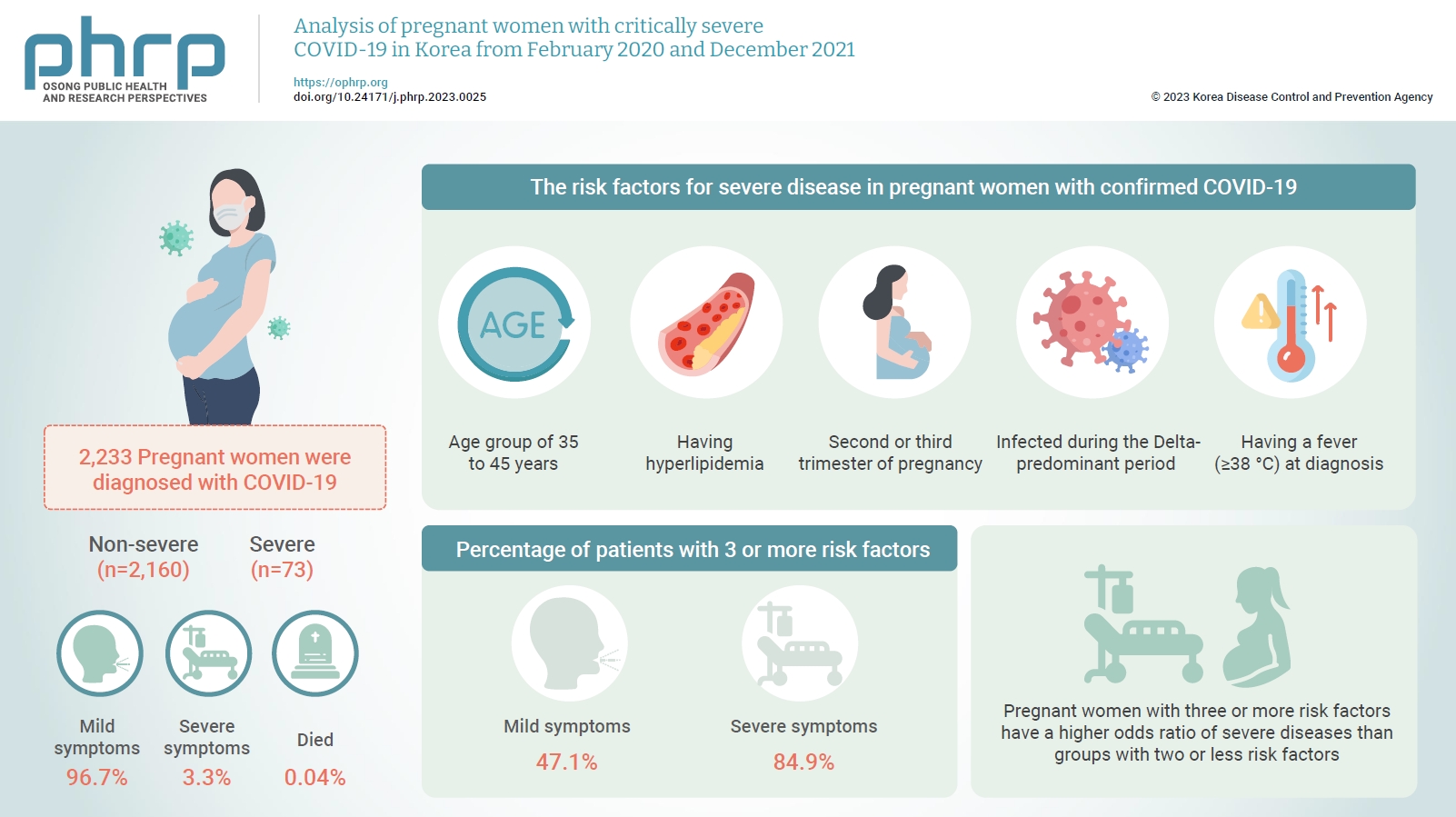
- Objectives
This study aimed to describe the characteristics and risk factors for severe disease in pregnant women infected with coronavirus disease 2019 (COVID-19) from the early days of the COVID-19 epidemic in Korea to the predominant period of the Delta variant.
Methods
A retrospective cohort study was conducted among pregnant women diagnosed with COVID-19 between February 2020 and December 2021. Logistic regression analysis was performed to compare severe and mild cases after adjusting for pregnant women’s age, nationality, infection route, outbreak area, infection period, symptoms, underlying disease, smoking status, trimester, and COVID-19 vaccination status.
Results
In total, 2,233 pregnant women were diagnosed with COVID-19 by December 2021. Among these, 96.7% had mild symptoms, 3.3% had severe symptoms, and 0.04% died. The risk factors for severe disease in pregnant women with confirmed COVID-19 were being in the age group of 35 to 45 years, having hyperlipidemia, being in the second or third trimester of pregnancy at the time of COVID-19 diagnosis, being infected during the Delta-predominant period, and having a fever (≥38 °C) at diagnosis. Furthermore, 47.1% of patients in the mild group and 84.9% of patients in the severe group had 3 or more risk factors.
Conclusion
Pregnant women with COVID-19 mainly experienced mild symptoms, but those with risk factors were at a higher risk of developing severe symptoms. Therefore, treatment and follow-up management should be thoroughly implemented.
Brief Report
- The effectiveness of Paxlovid treatment in long-term care facilities in South Korea during the outbreak of the Omicron variant of SARS-CoV-2
- Hanul Park, Young Joon Park, Hye Young Lee, Mi Yu, Yeong-Jun Song, Sang Eun Lee, Ji-Joo Lee, Eun-Sol Lee, Yeonjung Kim
- Osong Public Health Res Perspect. 2022;13(6):443-447. Published online December 23, 2022
- DOI: https://doi.org/10.24171/j.phrp.2022.0262
- 3,271 View
- 215 Download
- 7 Web of Science
- 9 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 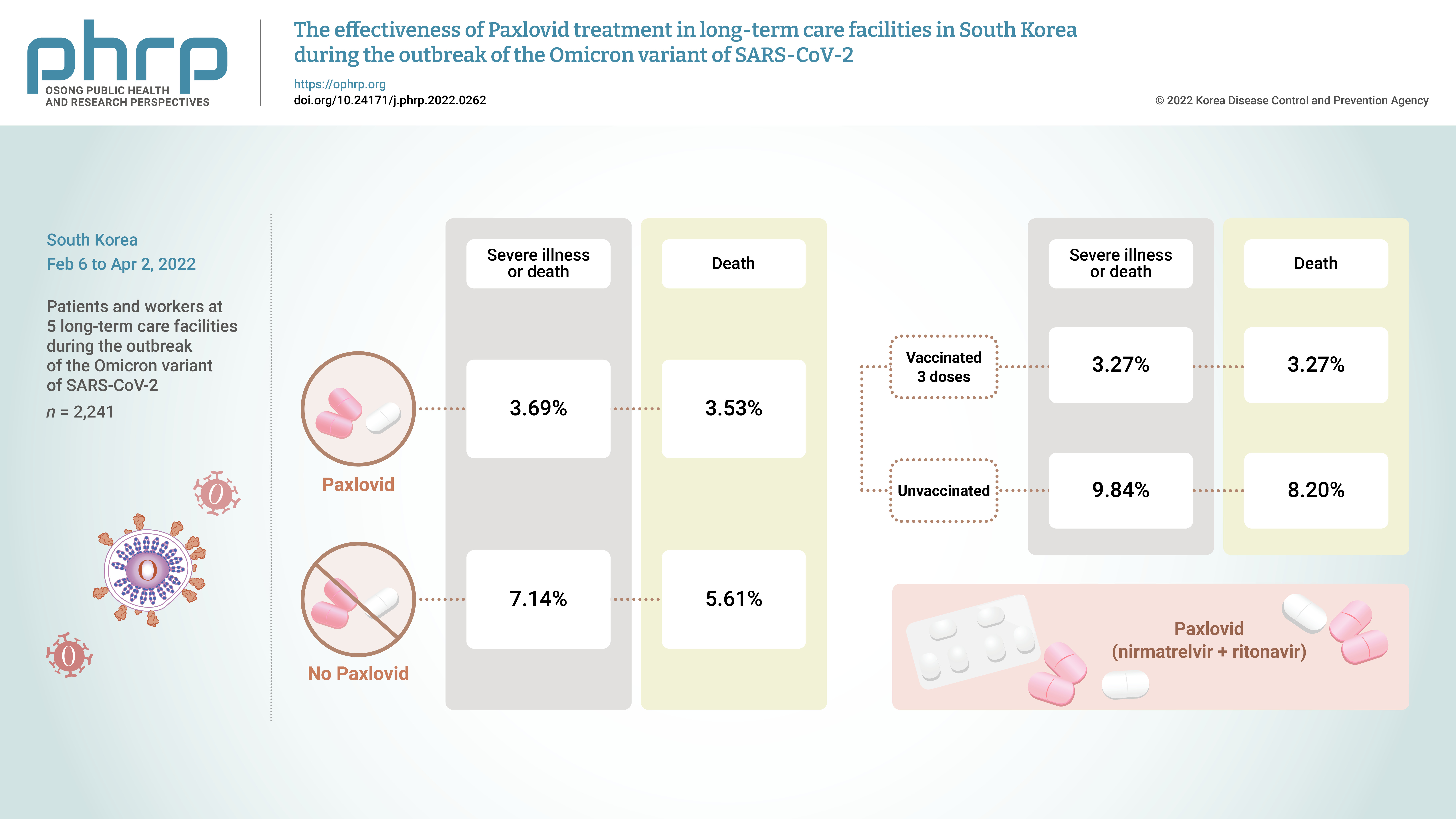
- Objectives
On November 5, 2021, Pfizer Inc. announced Paxlovid (nirmatrelvir +ritonavir) asa treatment method that could reduce the risk of hospitalization or death for patients withconfirmed coronavirus disease 2019 (COVID-19).Methods: From February 6, 2022 to April 2, 2022, the incidence of COVID-19 and the effectsof treatment with Paxlovid were analyzed in 2,241 patients and workers at 5 long-term carefacilities during the outbreak of the Omicron variant of severe acute respiratory syndromecoronavirus 2 in South Korea.Results: The rate of severe illness or death in the group given Paxlovid was 51% lower thanthat of the non-Paxlovid group (adjusted risk ratio [aRR], 0.49; 95% confidence interval [CI],0.24−0.98). Compared to unvaccinated patients, patients who had completed 3 doses of thevaccine had a 71% reduced rate of severe illness or death (aRR, 0.29; 95% CI, 0.13−0.64) and a65% reduced death rate (aRR, 0.35; 95% CI, 0.15−0.79).Conclusion: Patients given Paxlovid showed a lower rate of severe illness or death and alower fatality rate than those who did not receive Paxlovid. Patients who received 3 dosesof the vaccine had a lower rate of severe illness or death and a lower fatality rate than theunvaccinated group. -
Citations
Citations to this article as recorded by- Efficacy and safety of antiviral treatments for symptomatic COVID-19 outpatients: Systematic review and network meta-analysis
Meital Zur, Thalia Peselev, Stav Yanko, Victoria Rotshild, Ilan Matok
Antiviral Research.2024; 221: 105768. CrossRef - Clinical Effectiveness of Ritonavir-Boosted Nirmatrelvir—A Literature Review
Sydney Paltra, Tim O. F. Conrad
Advances in Respiratory Medicine.2024; 92(1): 66. CrossRef - Effectiveness of nirmatrelvir‐ritonavir on severe outcomes of COVID‐19 in the era of vaccination and Omicron: An updated meta‐analysis
Sien Ombelet, Diego Castanares‐Zapatero, Fabian Desimpel, Frank Hulstaert, Sabine Stordeur, Dominique Roberfroid
Journal of Medical Virology.2024;[Epub] CrossRef - COVID‐19 infection in patients with haematological malignancies: A single‐centre survey in the latest Omicron wave in China
Xiaolu Zhu, Qian Jiang, Jin Lu, Yuqian Sun, Xiaosu Zhao, Shenmiao Yang, Feifei Tang, Wenjing Yu, Ting Zhao, Xiaohong Liu, Jinsong Jia, Wenbing Duan, Lijuan Hu, Jing Wang, Yang Liu, Nan Peng, Xuelin Dou, Rui Ma, Qiang Fu, Huifang Wang, Kaiyan Liu, Xiaojun
British Journal of Haematology.2023; 202(1): 31. CrossRef - The association mental health of adolescents with economic impact during the COVID-19 pandemic: a 2020 Korean nationally representative survey
Hanul Park, Kang-Sook Lee
BMC Public Health.2023;[Epub] CrossRef - Efficacy and safety of paxlovid (nirmatrelvir/ritonavir) in the treatment of COVID‐19: An updated meta‐analysis and trial sequential analysis
Haokun Tian, Changsen Yang, Tiangang Song, Kechen Zhou, Lequan Wen, Ye Tian, Lirui Tang, Weikai Xu, Xinyuan Zhang
Reviews in Medical Virology.2023;[Epub] CrossRef - Real-World Effectiveness of Nirmatrelvir-Ritonavir and Its Acceptability in High-Risk COVID-19 Patients
Min-Kyung Kim, Kyung-Shin Lee, Sin Young Ham, Youn Young Choi, Eunyoung Lee, Seungjae Lee, Bora Lee, Jaehyun Jeon, BumSik Chin, Yeonjae Kim, Gayeon Kim, Hee-Chang Jang, Jae-Phil Choi, Sang-Won Park
Journal of Korean Medical Science.2023;[Epub] CrossRef - Effectiveness of Molnupiravir Treatment in Patients with COVID-19 in Korea: A Propensity Score Matched Study
Hye Rim Park, Min-Gyu Yoo, Jong Mu Kim, Soon Jong Bae, Hyungmin Lee, Jungyeon Kim
Infection & Chemotherapy.2023; 55(4): 490. CrossRef - Nirmatrelvir combined with ritonavir for preventing and treating COVID-19
Stefanie Reis, Maria-Inti Metzendorf, Rebecca Kuehn, Maria Popp, Ildiko Gagyor, Peter Kranke, Patrick Meybohm, Nicole Skoetz, Stephanie Weibel
Cochrane Database of Systematic Reviews.2023;[Epub] CrossRef
- Efficacy and safety of antiviral treatments for symptomatic COVID-19 outpatients: Systematic review and network meta-analysis
Original Article
- Depression among Korean Adults with Type 2 Diabetes Mellitus: Ansan-Community-Based Epidemiological Study
- Chan Young Park, So Young Kim, Jong Won Gil, Min Hee Park, Jong-Hyock Park, Yeonjung Kim
- Osong Public Health Res Perspect. 2015;6(4):224-232. Published online August 31, 2015
- DOI: https://doi.org/10.1016/j.phrp.2015.05.004
- 3,113 View
- 13 Download
- 22 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
There are an increasing number of studies being carried out on depression in patients with diabetes. Individuals with diabetes have been reported as having a higher prevalence of depression compared to those without diabetes. However, only a few studies involving Korean patients have been conducted. The aims of this study were to examine the prevalence of depression and to find various risk factors according to the degree of depression among Korean patients with Type 2 diabetes mellitus (T2DM).
Methods
An Ansan-community-based epidemiological study was conducted from 2005 to 2012. The total number of participants in this study was 3,540, from which patients with diabetes (n = 753) have been selected. The presence of depression was evaluated using the Beck Depression Inventory total score.
Results
The prevalence of depression was 28.8%. The mean age of participants was 55.5 ± 8.2 years. We divided the participants into three groups (without-depression, moderate-depression, and severe-depression groups) to examine the depression prevalence among Korean T2DM patients. The unemployed participants had 2.40 [95% confidence interval (CI) 1.21–4.76], the low-income participants had 2.57 (95% CI 1.52–4.35), the participants using an oral diabetes medicine or insulin had 2.03 (95% CI 1.25–3.32), the participants who are currently smoking had 2.03 (95% CI 1.10–3.73), and those without regular exercise had 1.91 (95% CI 1.17–3.14) times higher odds of depression in the severe-depression group, compared with the without-depression group.
Conclusion
There was a significant association between depression prevalence and diabetes, and we found various risk factors according to the degree of depression in Korean patients with T2DM. -
Citations
Citations to this article as recorded by- Psychological Health and Diabetes Self-Management among Patients with Type 2 Diabetes during COVID-19 in the Southwest of Saudi Arabia
Abdulrhman H. Alkhormi, Mohamed Salih Mahfouz, Najim Z. Alshahrani, Abdulrahman Hummadi, Wali A. Hakami, Doha H. Alattas, Hassan Q. Alhafaf, Leena E. Kardly, Mulook A. Mashhoor
Medicina.2022; 58(5): 675. CrossRef - Higher risk of depression in individuals with type 2 diabetes and obesity: Results of a meta-analysis
Thelma Beatriz González-Castro, Yudy Merady Escobar-Chan, Ana Fresan, María Lilia López-Narváez, Carlos Alfonso Tovilla-Zárate, Isela Esther Juárez-Rojop, Jorge L Ble-Castillo, Alma Delia Genis-Mendoza, Pedro Iván Arias-Vázquez
Journal of Health Psychology.2021; 26(9): 1404. CrossRef - The Effects of Meditation with a Biofeedback Program on Stress and Depression Levels among People with Mild Depression Diabetes
Ormanee Patarathipakorn, Manyat Ruchiwit, Marlaine Smith
The Open Public Health Journal.2021; 14(1): 104. CrossRef - Association between the level of adherence to dietary guidelines and depression among Korean patients with type 2 diabetes mellitus
Seonghee Park, Kyong Park
Journal of Psychosomatic Research.2021; 145: 110463. CrossRef - Depression Among Patients with Type 2 Diabetes Mellitus: Prevalence and Associated Factors in Hue City, Vietnam
Nhu Minh Hang Tran, Quang Ngoc Linh Nguyen, Thi Han Vo, Tran Tuan Anh Le, Ngoc Ha Ngo
Diabetes, Metabolic Syndrome and Obesity: Targets .2021; Volume 14: 505. CrossRef - Factors Associated with Depressive Symptoms in Korean Adults with Diabetes Mellitus: A Cross-Sectional Study
Mihyun Jeong
Healthcare.2021; 9(8): 1049. CrossRef - Spiritual intelligence, mindfulness, emotional dysregulation, depression relationship with mental well-being among persons with diabetes during COVID-19 pandemic
Wojujutari Kenni Ajele, Teslim Alabi Oladejo, Abimbola A. Akanni, Oyeyemi Bukola Babalola
Journal of Diabetes & Metabolic Disorders.2021; 20(2): 1705. CrossRef - Depression and Its Predictors among Diabetes Mellitus Patients Attending Treatment in Hawassa University Comprehensive Specialized Hospital, Southern Ethiopia
Bereket Beyene Gebre, Suzan Anand, Zebene Mekonnen Assefa
Journal of Diabetes Research.2020; 2020: 1. CrossRef - Effect of Study Design and Survey Instrument to Identify the Association Between Depressive Symptoms and Physical Activity in Type 2 Diabetes, 2000-2018: A Systematic Review
Jusung Lee, Timothy Callaghan, Marcia Ory, Hongwei Zhao, Margaret Foster, Jane N. Bolin
The Diabetes Educator.2020; 46(1): 28. CrossRef - Genetic Overlap Between Type 2 Diabetes and Depression in a Sri Lankan Population Twin Sample
Carol Kan, Kaushalya Jayaweera, Anushka Adikari, Sisira Siribaddana, Helena M.S. Zavos, Lisa Harber-Aschan, Athula Sumathipala, Matthew Hotopf, Khalida Ismail, Frühling Rijsdijk
Psychosomatic Medicine.2020; 82(2): 247. CrossRef - Depression in Iranian Children with Diabetes and Related Factors
Azadeh Sayarifard, Fatemeh Sayarifard, Maryam Nazari, Morteza Nikzadian, Mona Amrollahinia, Javad Mahmoudi-Gharaei
Iranian Journal of Pediatrics.2020;[Epub] CrossRef - Prevalence of Undiagnosed Depression in Patients With Type 2 Diabetes
Dina Siddiq Abdulhadi Alajmani, Amna Mohamad Alkaabi, Mariam Waleed Alhosani, Ayesha Abdulaziz Folad, Fawzia Ahmed Abdouli, Frederick Robert Carrick, Mahera Abdulrahman
Frontiers in Endocrinology.2019;[Epub] CrossRef - Risk and protective factors of co-morbid depression in patients with type 2 diabetes mellitus: a meta analysis
Aidibai Simayi, Patamu Mohemaiti
Endocrine Journal.2019; 66(9): 793. CrossRef - The prevalence of comorbid depression in patients with type 2 diabetes: an updated systematic review and meta-analysis on huge number of observational studies
Mohammad Khaledi, Fahimeh Haghighatdoost, Awat Feizi, Ashraf Aminorroaya
Acta Diabetologica.2019; 56(6): 631. CrossRef - Effect of walking and aerobic exercise on physical performance and depression in cases of type 2 diabetes mellitus
Manal K. Youssef
The Egyptian Journal of Internal Medicine.2019; 31(2): 142. CrossRef - Premorbid risk perception, lifestyle, adherence and coping strategies of people with diabetes mellitus: A phenomenological study in the Brong Ahafo Region of Ghana
Philip Teg-Nefaah Tabong, Vitalis Bawontuo, Doris Ningwiebe Dumah, Joseph Maaminu Kyilleh, Tolgou Yempabe, Noël C. Barengo
PLOS ONE.2018; 13(6): e0198915. CrossRef - Past and Current Status of Adult Type 2 Diabetes Mellitus Management in Korea: A National Health Insurance Service Database Analysis
Seung-Hyun Ko, Kyungdo Han, Yong-ho Lee, Junghyun Noh, Cheol-Young Park, Dae-Jung Kim, Chang Hee Jung, Ki-Up Lee, Kyung-Soo Ko
Diabetes & Metabolism Journal.2018; 42(2): 93. CrossRef - Why Early Psychological Attention for Type 2 Diabetics Could Contribute to Metabolic Control
Alfredo Briones-Aranda, Manuela Castellanos-Pérez, Raquel Gómez-Pliego
Romanian Journal of Diabetes Nutrition and Metabol.2018; 25(3): 329. CrossRef - Depression and Mortality in People with Type 2 Diabetes Mellitus, 2003 to 2013: A Nationwide Population-Based Cohort Study
Jong-Hyun Jeong, Yoo Hyun Um, Seung-Hyun Ko, Jong-Heon Park, Joong-Yeol Park, Kyungdo Han, Kyung-Soo Ko
Diabetes & Metabolism Journal.2017; 41(4): 296. CrossRef - Diabetes-related distress and its associated factors among patients with type 2 diabetes mellitus in China
Huanhuan Zhou, Junya Zhu, Lin Liu, Fan Li, Anne F. Fish, Tao Chen, Qingqing Lou
Psychiatry Research.2017; 252: 45. CrossRef - Comorbidity of depression and diabetes: an application of biopsychosocial model
Tesfa Dejenie Habtewold, Md. Atiqul Islam, Yosef Tsige Radie, Balewgizie Sileshi Tegegne
International Journal of Mental Health Systems.2016;[Epub] CrossRef - Differences in depression between unknown diabetes and known diabetes: results from China health and retirement longitudinal study
Huaqing Liu, Xiaoyue Xu, John J. Hall, Xuesen Wu, Min Zhang
International Psychogeriatrics.2016; 28(7): 1191. CrossRef
- Psychological Health and Diabetes Self-Management among Patients with Type 2 Diabetes during COVID-19 in the Southwest of Saudi Arabia
Article
- Dietary Patterns and Osteoporosis Risk in Postmenopausal Korean Women
- Seon-Joo Park, Seong-Eun Joo, Haesook Min, Jae Kyung Park, Yeonjung Kim, Sung Soo Kim, Younjhin Ahn
- Osong Public Health Res Perspect. 2012;3(4):199-205. Published online December 31, 2012
- DOI: https://doi.org/10.1016/j.phrp.2012.10.005
- 2,978 View
- 18 Download
- 28 Crossref
-
 Abstract
Abstract
 PDF
PDF - Objectives
The prevalence of osteoporosis and related fractures has increased rapidly in Korean women. Proper nutrition intake is associated with the prevention of osteoporosis. We analyzed the association between dietary patterns and the risk of osteoporosis during a 4-year follow-up in postmenopausal Korean women.
Methods
Postmenopausal women (n = 1,725) who participated in the Korean Genome and Epidemiology Study were enrolled. Food intake was assessed using a validated semiquantitative food frequency questionnaire, and a quantitative ultrasound device was used to measure the speed of sound at the radius and tibia.
Results
Three major dietary patterns were identified using factor analysis based on baseline intake data: traditional (high intake of rice, kimchi, and vegetables), dairy (high intake of milk, dairy products, and green tea), and western (high intake of sugar, fat, and bread). Multivariate Cox proportional hazards models were used to estimate relative risk for osteoporosis. An inverse association was detected between the dairy dietary pattern and the osteoporosis incidence [relative risk (RR): 0.63, 95% confidence interval (CI): 0.42–0.93, p-trend=0.055 in radius; RR: 0.56, 95% CI: 0.35–0.90, p-trend=0.048 in tibia]. Individuals in the highest quintile for the traditional dietary pattern (p-trend = 0.009 in tibia) and western dietary pattern (p-trend = 0.043 in radius) demonstrated a higher risk of osteoporosis incidence than those in the lowest quintile.
Conclusion
These results suggested that high consumption of milk, dairy products, and green tea may reduce the risk of osteoporosis in postmenopausal Korean women. -
Citations
Citations to this article as recorded by- Identification of the Risk Factors Associated with Low Bone Density in Peri- and Early Postmenopausal Women
Dave B. Patel, Briana M. Nosal, Manije Darooghegi Mofrad, Ock K. Chun
Dietetics.2024; 3(1): 75. CrossRef - Dietary patterns associated with the risk of osteoporosis in postmenopausal women
Reema F. Tayyem, Rawan Ajeen, Amal Al-Khammash
Food Production, Processing and Nutrition.2023;[Epub] CrossRef - The Influence of the Mediterranean Dietary Pattern on Osteoporosis and Sarcopenia
María Carmen Andreo-López, Victoria Contreras-Bolívar, Beatriz García-Fontana, Cristina García-Fontana, Manuel Muñoz-Torres
Nutrients.2023; 15(14): 3224. CrossRef - Lifestyle and Dietary Patterns as Risk Factors for Osteoporosis:
A Literature Review
Reema Tayyem, Haya Abuhijleh, Amal Al-Khammash
Current Nutrition & Food Science.2023; 19(8): 806. CrossRef - Association between macronutrients intake distribution and bone mineral density
Shihua Gao, Xin Qian, Sicong Huang, Wanxi Deng, Zhe Li, Yingyu Hu
Clinical Nutrition.2022; 41(8): 1689. CrossRef - Drinking tea before menopause is associated with higher bone mineral density in postmenopausal women
Saili Ni, Lu Wang, Guowei Wang, Jie Lin, Yiyun Ma, Xueyin Zhao, Yuan Ru, Weifang Zheng, Xiaohui Zhang, Shankuan Zhu
European Journal of Clinical Nutrition.2021; 75(10): 1454. CrossRef - The relationship between healthy lifestyles and bone health
Bin Sheng, Xin Li, Andreas K. Nussler, Sheng Zhu
Medicine.2021; 100(8): e24684. CrossRef - Postmenopausal women with osteoporosis consume high amounts of vegetables but insufficient dairy products and calcium to benefit from their virtues: the CoLaus/OsteoLaus cohort
A. Lanyan, P. Marques-Vidal, E. Gonzalez-Rodriguez, D. Hans, O. Lamy
Osteoporosis International.2020; 31(5): 875. CrossRef - Combining Population-Specific Dietary Patterns in Meta-analyses: True or False?
Asma Salari-Moghaddam, Bagher Larijani, Ahmad Esmaillzadeh
Advances in Nutrition.2020; 11(2): 463. CrossRef - Effect of nutrient intake and dietary diversity score on osteoporosis of middle-aged adults and elderly based on 2015–2017 Korean National Health and Nutrition Examination Survey data
Sehyug Kwon, Jung Sug Lee
Journal of Nutrition and Health.2020; 53(2): 155. CrossRef - Reply to A Salari-Moghaddam et al.
Roberto Fabiani, Giulia Naldini, Manuela Chiavarini
Advances in Nutrition.2020; 11(3): 743. CrossRef - Repertoire of Structure–Activity-Based Novel Modified Peptides Elicits Enhanced Osteogenic Potential
Divya Upadhyay, Taruneet Kaur, Rajeev Kapila, Suman Kapila
Journal of Agricultural and Food Chemistry.2020; 68(31): 8308. CrossRef - Nutrient and Dietary Patterns in Relation to the Pathogenesis of Postmenopausal Osteoporosis—A Literature Review
Bolaji Lilian Ilesanmi-Oyelere, Marlena C. Kruger
Life.2020; 10(10): 220. CrossRef - Dietary Patterns, Body Composition, and Bone Health in New Zealand Postmenopausal Women
Bolaji L. Ilesanmi-Oyelere, Jane Coad, Nicole C. Roy, Marlena C. Kruger
Frontiers in Nutrition.2020;[Epub] CrossRef - Development of a Mobility Diet Score (MDS) and Associations With Bone Mineral Density and Muscle Function in Older Adults
Simon Rønnow Schacht, Mads Vendelbo Lind, Kenneth Hudlebusch Mertz, Jacob Bülow, Rasmus Bechshøft, Grith Højfeldt, Aide Schucany, Morten Hjulmand, Chiara Sidoli, Søren Binder Andersen, Mikkel Jensen, Søren Reitelseder, Lars Holm, Inge Tetens
Frontiers in Nutrition.2019;[Epub] CrossRef - Dietary Patterns in Relation to Low Bone Mineral Density and Fracture Risk: A Systematic Review and Meta-Analysis
Roberto Fabiani, Giulia Naldini, Manuela Chiavarini
Advances in Nutrition.2019; 10(2): 219. CrossRef - Dietary Patterns, Bone Mineral Density, and Risk of Fractures: A Systematic Review and Meta-Analysis
Edgar Denova-Gutiérrez, Lucía Méndez-Sánchez, Paloma Muñoz-Aguirre, Katherine Tucker, Patricia Clark
Nutrients.2018; 10(12): 1922. CrossRef - Pu-erh Tea Extract Ameliorates Ovariectomy-Induced Osteoporosis in Rats and Suppresses Osteoclastogenesis In Vitro
Titi Liu, Shihua Ding, Dan Yin, Xiangdan Cuan, Chuanqi Xie, Huanhuan Xu, Xuanjun Wang, Jun Sheng
Frontiers in Pharmacology.2017;[Epub] CrossRef - Association between Dietary Carotenoid Intake and Bone Mineral Density in Korean Adults Aged 30–75 Years Using Data from the Fourth and Fifth Korean National Health and Nutrition Examination Surveys (2008–2011)
Gebereamanuel Regu, Hyesook Kim, You Kim, Ju Paek, Gunjeong Lee, Namsoo Chang, Oran Kwon
Nutrients.2017; 9(9): 1025. CrossRef - Association between Dietary Patterns of Meat and Fish Consumption with Bone Mineral Density or Fracture Risk: A Systematic Literature
Simone Perna, Ilaria Avanzato, Mara Nichetti, Giuseppe D’Antona, Massimo Negro, Mariangela Rondanelli
Nutrients.2017; 9(9): 1029. CrossRef - Prospective Associations of Dietary and Nutrient Patterns with Fracture Risk: A 20-Year Follow-Up Study
Yohannes Melaku, Tiffany Gill, Sarah Appleton, Anne Taylor, Robert Adams, Zumin Shi
Nutrients.2017; 9(11): 1198. CrossRef - Fat, Sugar, and Bone Health: A Complex Relationship
Li Tian, Xijie Yu
Nutrients.2017; 9(5): 506. CrossRef - Lactobacillus reuteri can Improve BMD in Patients Having Bone Fragility
Moetazza M. Alshafe, Seham S. Kassem, Azzat B. El-Khal, Mohamed T. Fouad, Enas N. Danial, Emtenan M. Hanafi, Maha M. Saber, Eitedal M. Daoud
International Journal of Dairy Science.2017; 12(2): 143. CrossRef - Current Evidence on the Association of Dietary Patterns and Bone Health: A Scoping Review
Elham Z Movassagh, Hassan Vatanparast
Advances in Nutrition.2017; 8(1): 1. CrossRef - Dietary patterns and bone mineral density in Brazilian postmenopausal women with osteoporosis: a cross-sectional study
N A G de França, M B R Camargo, M Lazaretti-Castro, B S E Peters, L A Martini
European Journal of Clinical Nutrition.2016; 70(1): 85. CrossRef - Relationship between bone mineral density and dietary intake of β-carotene, vitamin C, zinc and vegetables in postmenopausal Korean women: a cross-sectional study
Da Eun Kim, Soo Hyun Cho, Hyoung Moo Park, Yu Kyung Chang
Journal of International Medical Research.2016; 44(5): 1103. CrossRef - Promoting osteoblast differentiation by the flavanes from Huangshan Maofeng tea is linked to a reduction of oxidative stress
Xiaobin Zeng, Jun Tian, Kangyong Cai, Xin Wu, Yang Wang, Yayuan Zheng, Yanjie Su, Liao Cui
Phytomedicine.2014; 21(3): 217. CrossRef - The association of dietary quality and food group intake patterns with bone health status among Korean postmenopausal women: a study using the 2010 Korean National Health and Nutrition Examination Survey Data
Gyeongah Go, Zuunnast Tserendejid, Youngsook Lim, Soyeon Jung, Younghee Min, Haeryun Park
Nutrition Research and Practice.2014; 8(6): 662. CrossRef
- Identification of the Risk Factors Associated with Low Bone Density in Peri- and Early Postmenopausal Women
Original Article
- Plasma Calcium and Risk of Hypertension: Propensity Score Analysis Using Data From the Korean Genome and Epidemiology Study
- Jong Wook Kim, Kwang-Pil Ko, Hee Jo Koo, Younjhin Ahn, Seon-Joo Park, Hyo-Mi Kim, Yeonjung Kim, Sung Soo Kim
- Osong Public Health Res Perspect. 2011;2(2):83-88. Published online June 30, 2011
- DOI: https://doi.org/10.1016/j.phrp.2011.07.004
- 2,789 View
- 13 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Objective
To investigate associations between plasma calcium and future incidence of hypertension in a healthy population.
Methods
We used prospective data from Ansung and Ansan cohorts (n = 10,038) of the Korean Genome and Epidemiology Study. Data from baseline (2001–02) to the fourth study (2007–08) were used. After excluding hypertensive cases at baseline, missing data, and outliers, 5560 participants were analyzed. Propensity scores for having higher plasma calcium (≥2.37 mmol/L) were created for each participant. After propensity score matching (1:1 nearest neighbor matching within caliper), 2153 pairs were left for analysis. Factors that were significantly different between the lower and higher plasma calcium groups before matching either became nonsignificant or the difference decreased in size.
Results
Using multivariable Cox proportional hazard models with robust standard errors accounting for clustering of matched pairs, higher plasma calcium was associated with higher incidence of hypertension (adjusted HR, 1.24; robust 95%CI, 1.07–1.43). Among those with higher plasma calcium, low dietary calcium intake increased the development of hypertension, but the effect was not significant. Sensitivity analysis showed that our results were robust to hidden bias.
Conclusions
Plasma calcium was positively associated with incidence of hypertension. These results expand on cross-sectional associations between hypercalcemia and the metabolic syndrome, and extend the link to future risk of hypertension. -
Citations
Citations to this article as recorded by- Hypocalcemia is associated with severe COVID-19: A systematic review and meta-analysis
Januar Wibawa Martha, Arief Wibowo, Raymond Pranata
Diabetes & Metabolic Syndrome: Clinical Research &.2021; 15(1): 337. CrossRef - Plasma total calcium concentration is associated with blood pressure and systemic vascular resistance in normotensive and never-treated hypertensive subjects
Lasse Oinonen, Jenni Koskela, Arttu Eräranta, Antti Tikkakoski, Mika Kähönen, Onni Niemelä, Jukka Mustonen, Ilkka Pörsti
Blood Pressure.2020; 29(3): 137. CrossRef - Hipercalcemia como causa de hipertensión arterial presentación de un caso
Carlos Harrison Gómez, Derek Harrison Ragle, Francisco Sánchez Lezama, Adalberto Arceo Navarro, Víctor Manuel Arredondo Arzola, Luis Gerardo Domínguez Carrillo
Atención Familiar.2017;[Epub] CrossRef
- Hypocalcemia is associated with severe COVID-19: A systematic review and meta-analysis



 First
First Prev
Prev


